Living life in your 20s and 30s seems pretty straightforward. You can eat what you want for the most part, don’t need to exercise to stay healthy (kind of), and you can stay out all night if you wish to, and your body seems to bounce back faster than a rubber ball. You’re basically an invincible weekend warrior that nothing and no one can stop.
But as you get older, you realize that the things that flew when you were 20 don’t fly so well anymore. That one night of lost sleep leaves you feeling crappy for a week, or maybe the chocolates you’ve been munching on have gone straight to your hips.
Women entering their 50s are at a completely different stage of life, and you may notice some significant health changes, especially as menopause looms on the horizon. And because of this, nutrient needs also change. You may need more of something that wasn’t so important 10 or 20 years ago.
In lieu of that, we’re giving you a rundown of some reasons women in their 50s have different nutritional needs than younger women and the daily nutrient essentials you should look for.
The Focus For Women In Their 50s
Changing levels of estrogen and progesterone that come into play with menopause can mean a lot of changes for women in their 50s, both in terms of physical and physiological changes.
Maintaining Muscle Mass
Would you believe us if we told you that after the age of 30, the average adult loses about 3-8% of their muscle mass each decade? 1
Other studies show that this number may not be as drastic, with most people losing muscle mass at an annual rate of approximately 1 to 2%, and strength declining at roughly 1.5% per year but can accelerate to as much as 3% per year after the age of 60 2.
The loss of muscle associated with aging is called sarcopenia, and it’s thought to reflect mainly an age-related decrease in muscle protein synthesis rather than an excess catabolic process linked to disease or reduced caloric intake.
However, some research suggests that low-grade chronic inflammation with increased protein degradation may contribute.
Building Healthy Bones
As estrogen levels start to drop, it can spell trouble for bone health if you don’t keep on top of it. That’s because estrogen is a major regulator of bone metabolism in women and is needed for proper growth and maturation of bone, along with regulating bone turnover 3.
However, because there is a loss of ovarian estrogens during menopause, it results in a drop in bone mineral density, weakened bones, and an increased risk of fractures and osteoporosis.
Metabolism
As much as we’d love for our metabolism to stay revved well into our 90s, the natural course of aging doesn’t follow the same logic, and as a result, packing on the pounds becomes that much easier. There are a few reasons why:
- People tend to be less physically active as they age
- Muscle loss declines after 30, and muscle accounts for a large percentage of energy expenditure
- Mitochondria, the powerhouses of your cells, become less efficient with age
Hormone Balance
For many women, hormones are all over the place throughout their entire life, but menopause represents a bit of a special time as it marks the cessation of menstruation and massive fluctuations in estrogen levels 4.
These fluctuations are why many women, even in their early 50s, start to experience symptoms of perimenopause, such as hot flashes, vaginal dryness, menstrual irregularities, weight gain, and others.
During this time, it’s key to provide your body with the nutrients it needs to support hormonal balance and support detoxification pathways that eliminate excess hormones and thyroid function, which controls your metabolism and thermoregulation.
Top 5 Vitamins For Women In Their 50s
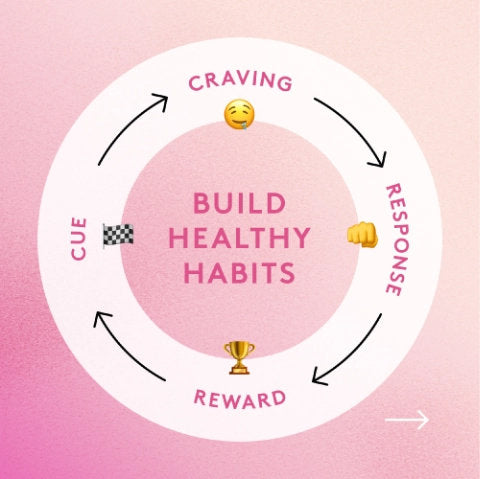
With all that said, getting sufficient nutrients is key to maintaining health during aging and limiting the impacts of the factors we just mentioned. So, what nutrients should you be looking for?
1. Calcium
With estrogen levels declining and exhibiting such a profound impact on bone health, calcium is one nutrient you’ll want to make sure you’re getting enough of to maintain strong bones.
Calcium is needed for several functions in the body, of which skeletal mineralization is perhaps the most important. Bone is mineralized connective tissue, and calcium represents one of the major components, meaning that adequate levels are crucial for bone strength and structure 5.
Studies suggest that adequate calcium intake, in the presence of adequate vitamin D, has been shown to prevent bone loss and reduce the risk of fractures in peri-and postmenopausal women 6.
And although calcium isn’t as effective as antiresorptive agents like estrogen, it plays an essential role in mitigating bone loss. For women over 50, the recommended dose of calcium is 1,200 mg alongside at least 400-600 IU of vitamin D 5.
However, be mindful of larger doses of calcium, as it can interfere with the absorption of other key nutrients.
2. Vitamin D + K2
Vitamin D is arguably one of the most important vitamins in the body and even more so for women entering their 50s due to its role in supporting calcium absorption. It’s estimated that approximately 90% of adults between 51 and 70 years old aren’t getting sufficient amounts of vitamin D in their diet 7.
Without sufficient vitamin D levels, the body cannot form enough of the hormone calcitriol, which leads to insufficient calcium absorption from the diet. In cases like this, the body reverts to pulling calcium from skeletal stores, which weakens existing bone and prevents the formation of new, stronger bones.
Vitamin D also supports the production of vitamin K-dependent proteins, which require vitamin K for carboxylation to function properly 8. These vitamin-K-dependent proteins regulate the activity of matrix Gla protein (MGP) and osteocalcin (bone Gla protein), and insufficient levels of vitamin K have been associated with an increased risk of osteoporosis.
Besides its role in calcium homeostasis, vitamin D is also needed to support immune function, mood (which we all know can be a little wonky with hormonal imbalances), heart health, muscle mass, and regulating inflammation.
3. Magnesium
Magnesium is a hugely underappreciated nutrient involved in over 300 biochemical reactions in the body. It plays a vital role in muscle contraction, mood, bone health, hormones, sleep, and more.
But for women in their 50s going through menopause, magnesium plays a critical role in supporting bone health. Roughly 60% of magnesium stops are found in bone and are essential in preventing osteoporosis.
Bones naturally undergo a remodeling process called osteogenesis that serves to increase strength and structure. During this process, bones are broken down by osteoclasts and rebuilt by osteoblasts.
However, because estrogen levels decline around menopause, there is a spike in osteoclast activity, potentially resulting in major bone loss. As a result, bones are being broken down faster than they’re being rebuilt, leading to weakened, porous bones 9.
The reason magnesium becomes increasingly important here is its role in cartilage and bone matrix calcification. Low magnesium levels have also been linked to lower activity of parathyroid hormone (PTH) and vitamin D, both of which are essential for proper bone development 10.
Also, magnesium deficiency has been shown to decrease osteoblast activity and increase inflammation, contributing to weaker bones over time.
Magnesium is also great for supporting sleep, which can suffer if women are experiencing more severe menopause symptoms, like hot flashes, that keep them up at night.
4. Vitamin B12
Vitamin B12 is an essential nutrient needed for forming red blood cells, which plays a significant role in energy production. However, for B12 to be absorbed from the diet, it requires something called intrinsic factor (IF), which is activated by stomach acid. Because levels of stomach acid and IF tend to decline with age, absorption of B12 can suffer.
And if you’re consuming a plant-based diet with insufficient amounts of B12 to begin with, it can lead to even lower levels. Inadequate levels of B12 not only affect hematopoiesis and energy levels, but they can also lead to anemia, a common blood disorder characterized by fatigue.
5. Omega-3s
While there’s no magic pill that will stop the nasty effects of aging on the body, omega-3s are about as close as you can get. Want lustrous, healthy skin, hair, and nails? Try omega-3s. Want better eyesight? Omega-3s. More favorable cholesterol levels? You guessed it, try omega-3s.
Omega-3 fatty acids are some of the most critical nutrients we can give our bodies that play a role in everything from promoting proper nerve function and producing hormones, to keeping levels of inflammation at bay.
Some studies also suggest that omega-3s can help provide relief from symptoms of menopause. Research finds that depression and hot flashes commonly co-occur during the transition to menopause, and women experiencing hot flashes are at increased risk for major depressive disorder (MDD) 11.
Typically, conventional antidepressants have been used in treatment for both the mood and vasomotor symptoms (VMS) in perimenopausal and postmenopausal women, but many women are reluctant to use these due to the hefty list of side effects.
However, omega-3 fatty acids have been shown to affect serotonergic transmission, mitigating VMS and reducing depressive symptoms 11.
PL-NutriGenesis Multi: Your Lock And Key For Maintaining Health Into Your 50s

Performance Lab NutriGenesis Multi for Women is like no other multivitamin on the market. It’s an ultramodern supplement designed to restore depleted nutrient levels for overall health and optimal whole-body performance.
Containing 100% of the RDI of more than 17+ essential vitamins and minerals, NutriGenesis Multi for Women is precisely calibrated to support women’s specific nutritional needs and hormonal balance.
It’s not a generic, one-size-fits-all multi that you’ll find on supermarket shelves. It’s created using ultramodern nutrition technology unique to Performance Lab®.
The nutrients in Multi are bioengineered with cofactors that boost absorption and maximize benefits, all delivered in NutriCaps®—Prebiotic-infused and vegan-friendly capsules for digestive comfort and peace of mind.
Just one capsule daily is all you need for optimal body performance, whether you’re going through perimenopause, in the thick of menopause, or past it. They’re designed to support you from every angle.
References
- KL English, D Paddon-Jones. Protecting muscle mass and function in older adults during bed rest. Curr Opin Clin Nutr Metab Care. 2010;13(1):34-39.
- Y Rolland, S Czerwinski, G Abellan Van Kan, et al. Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives.J Nutr Health Aging. 2008;12(7):433-450.
- HK Väänänen, PL Härkö Estrogen and bone metabolism.Maturitas. 1996;23 Suppl:S65-S69.
- JC Perimenopause: the complex endocrinology of the menopausal transition. Endocr Rev. 1998;19(4):397-428.
- L Vannucci, C Fossi, S Quattrini, et al. Calcium Intake in Bone Health: A Focus on Calcium-Rich Mineral Waters. Nutrients. 2018;10(12):1930.
- North American Menopause Society. The role of calcium in peri- and postmenopausal women: consensus opinion of The North American Menopause Society. 2001;8(2):84-95.
- JA Sunyecz. The use of calcium and vitamin D in the management of osteoporosis.Ther Clin Risk Manag. 2008;4(4):827-836.
- AJ van Ballegooijen, S Pilz, A Tomaschitz, MR Grübler, N Verheyen. The Synergistic Interplay between Vitamins D and K for Bone and Cardiovascular Health: A Narrative Review.Int J Endocrinol. 2017;2017:7454376.
- K Peacock, KM Ketvertis. Menopause. (Updated 2021 Jun 29). In: StatPearls (Internet). Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507826/
- S Castiglioni, A Cazzaniga, W Albisetti, JA Maier. Magnesium and osteoporosis: current state of knowledge and future research directions. 2013;5(8):3022-3033.
- MP Freeman, JR Hibbeln, M Silver, et al. Omega-3 fatty acids for major depressive disorder associated with the menopausal transition: a preliminary open trial. 2011;18(3):279-284.