From supporting digestion and immune function to mental health and weight management, the gut plays a big (and undercover) role in your health. Apart from eating well, sleep, exercise, and probiotics are some of the easiest ways to take care of it.
Your gut is always talking. Whether it’s growing to signify it's hungry or you’re getting butterflies before stepping on stage, the gut is smart—and it’s highly responsive to its environment.
The gastrointestinal tract (GI), sometimes referred to as the digestive tract, can be used as one of the most important barometers of health.
More than 70% of your immune system resides in your gut, and roughly 90% of all serotonin, an important neurotransmitter, is synthesized there, too 1. While an unhealthy gut affects digestion, it also affects a lot more—immunity, mood, weight regulation, cognitive function, and more.
With a bit of TLC, you can turn your gut health around and optimize your performance. Diet and supplementation are all great starting points, but lifestyle factors play a significant role, too.
So, we’re diving into all things gut health and giving you the scoop on why it’s important, the signs and symptoms of an unhealthy gut, and what to do about it.
Ready to get your gut back on track? Let’s get started.
Bacteria and your health
There’s no shortage of health topics on the horizon for discussion, but one of the biggest and most recent is all about gut health—the gut microbiome.
The human body is home to trillions of microbes that make up a mini-ecosystem in the digestive tract that help us to break down food and absorb its nutrients 2. Generally speaking, that’s about where we think the function of the gut stops—but it’s far from that.
Recent studies show that the bacteria that inhabit your gut affect things far beyond digestion, ranging from inflammation and fat loss to cognitive function, mood disorders, and even aging 3-5. The more we study, the more we realize how interconnected the gut is with virtually every system in the body.
The gut bacteria produce digestive enzymes and nutrients that support optimal health and well-being, and they can even influence things like metabolic rate and weight regulation.
But perhaps one of the biggest connections for gut health is with the immune system. Roughly 70-80% of your immune system resides in your gut, which means having a healthy gut with high microbial diversity is key for healthy and balanced immune responses 6.
Related Post: Gut Health and Weight Loss: How Your Gut Bacteria Can Influence Your Weight
The Gut-Brain Connection
Have you ever had an intense food craving that you get in your car to head out for a midnight fast-food taco run? Or a pint of your favorite ice cream? Your gut has a lot of control over your food choices, but as it turns out, it can also heavily influence your mood and behavior.
We’ve known about the link between gut health and mental health since the early 1900s, but recently, we're more interested in how gut health affects mental health disorders. This renewed interest has unveiled the close relationship between gut health and behavioral issues, mood, and gut bacteria imbalances.
But it’s more than just diet that influences a healthy gut.
Without diving too much into the science of it all, your gut and brain are connected in three ways:
- The vagus nerve
- The enteric nervous system (ENS)
- Gut-brain axis
Let’s look into those.
The vagus nerve is the tenth cranial nerve and the longest nerve in the body.
Running from your brain stem through the neck, thorax, and abdomen, it supplies motor parasympathetic nerve fibers to all the organs except the adrenal glands. It regulates digestion, heart rate, respiratory rate, vasomotor activity, and specific reflex actions (coughing, sneezing, swallowing, vomiting) 7.
The enteric nervous system (ENS), also known as the second brain, connects to the central nervous system and contains sensory neurons in the gut wall.
The neural circuits of the ENS control motor functions, local blood flow, mucosal transport, and secretions, and modulate various immune and endocrine functions 8. Dysfunctions of the ENS often result in digestive disorders.
The gut-brain axis is a bidirectional axis between the central and the enteric nervous system, linking the emotional and cognitive centers of the brain with intestinal functions 9. This link is why mental or emotional stress levels can profoundly influence digestive function.
There’s a lot we can say about the importance of gut health, but some of the most profound links can be seen with anxiety and depression. The gut microbiota heavily influences the production of serotonin and dopamine—the “feel good” neurotransmitters.
Not only is serotonin a key player in mood, but it also regulates gastrointestinal motility. The ENS (remember, the link between the gut and the brain) uses over 30 neurotransmitters, including serotonin, dopamine, and acetylcholine 10.
Here’s an excellent example of the link between mood and gut health.
A 2011 study published in the British Journal of Nutrition looked at the effect of probiotic supplementation on anxiolytic-like activity in rats and the possible effects on anxiety, depression, stress, and coping strategies in humans 11.
Results showed that probiotics significantly decreased both the rats’ anxiety-like symptoms and the humans’ levels of anger, distress, hostility, and depression.
Other research shows that supplements designed to increase the diversity and number of healthy gut bacteria may improve anxiety symptoms and alter emotional information processing 12.
The Top 9 Signs And Symptoms Of Poor Gut Health
There’s no denying that diet plays a significant role in the microbial composition and health of the gut.
Still, several other components of modern-day life can influence gut health and the microbiome, including:
- High-stress levels
- Sleep deprivation
- Diet high in sugar and processed/refined carbohydrates
- Antibiotic use
- Inactivity/sedentary lifestyle
- All of these factors can affect other aspects of your health, including:
- Immune system function
- Hormone balance
- Weight management
- Chronic disease risk
- Cognitive function
You'll likely have symptoms if you’re struggling with dysbiosis or poor gut health. Here are ten common signs of an unhealthy gut:
- Digestive discomfort (gas, bloating, diarrhea, constipation, heartburn)
- Inflammation
- A high-sugar diet (or high in refined carbohydrates)
- Unintentional weight gain or weight loss
- Sleep disruptions
- Chronic fatigue
- Skin issues (psoriasis, eczema)
- Autoimmune diseases
- Food allergies, food intolerances, or sensitivities (causes symptoms like gas, bloating, diarrhea, nausea, and stomach pain)
- Brain fog/lack of mental clarity
What you can do to optimize gut health and balance gut bacteria
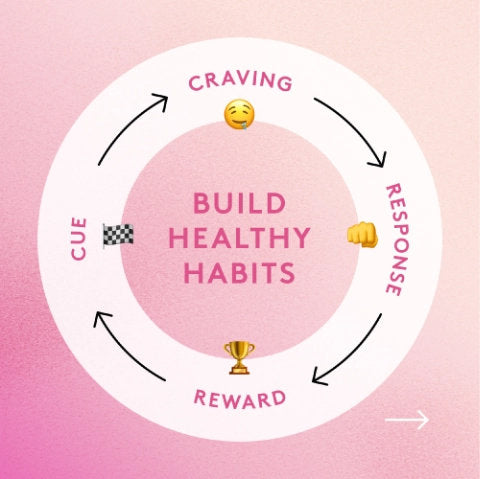
Ready to improve gut health? It might sound like a simple job, but let us tell you that it takes consistency, dedication, and work.
Your gut didn’t get to an unhealthy state overnight, and it’s not going to get to a healthy one that way, either. But here’s the thing: it is possible with a few simple diet and lifestyle tweaks.
Here are our top tips for reclaiming your gut health and living your best life:
Log your meals
Keeping track of your food is never ideal, but most people are largely unaware of what passes their lips—and food is a direct cause of an unhealthy gut. Writing down what you eat can help you take notice of how it affects how you feel afterward.
Oftentimes, it can help people identify food intolerances. Most people are surprised to find that tracking their food helps them identify issues that lead to GI problems—and gives them a much clearer picture of certain foods to eliminate from their diet.
Eat more fiber
Fiber is critical not only for regulating bowel movements but also for the health of your gut. Inside the gut, you’ll find millions of beneficial bacteria that offer numerous benefits to the body.
But without food, these gut bacteria cannot thrive and offer these benefits. That’s where fiber comes into the picture— a specific type of fiber called prebiotics.
They’re a “selectively fermented ingredient that allows specific changes, both in the composition and activity in the gastrointestinal microflora that confers benefits upon host well-being and health” 13.
Related Post: Should I Take Fiber Before or After a Meal?
In simple terms, prebiotic fiber feeds the beneficial bacteria in your gut, allowing them to thrive and proliferate, and preventing bad bacteria from taking over. Adding a fiber supplement like Performance Lab Prebiotic is a great way to support gut health.
Still, on top of that, you also need to focus on consuming a diet of whole, high-fiber foods like fruits, vegetables, beans and legumes, whole grains, and prebiotic-rich foods like garlic, onions, leeks, and oats.
More variety in your diet means more variety in your gut!
Limit your consumption of inflammatory foods
We know what you’re thinking, “what foods are inflammatory?” The Western diet—high in sugar, starch, and saturated and trans fat—is incredibly inflammatory 14.
The biggest culprits can alter the gut's microbial community and its functions, and a disruption to the microbial balance, also called dysbiosis, is a major contributor to gut inflammation and immune responses 15.
On top of gut inflammation, these foods have also been linked to various chronic diseases, including diabetes, obesity, cardiovascular diseases, and leaky gut 16. But the primary link between the Western diet and chronic diseases is inflammation.
So, when you limit your consumption of certain foods that trigger inflammation in the intestinal tract, you’re reducing systemic inflammation and disease risk and improving the environment and health of your gut by supporting the growth of beneficial bacteria.
Eat fermented foods (and invest in a probiotic supplement)
Fermented foods aren’t all created equal, but things like kimchi, tempeh, and miso are excellent sources of probiotic bacteria and can help increase good bacteria and eliminate harmful bacteria, but you want to ensure the product contains “live active cultures.”
If not found in the fridge, they’re likely not alive and will not provide benefits for gut health and the gut microbiome.
The thing with fermented foods is that they can be a bit funky tasting and aren’t for everyone. If you're not a fan of the probiotic-rich foods, investing in a prebiotic + probiotic supplement might be worth the money—but note that there is no magic pill.
Keeping the same diet and adding in a probiotic isn’t going to cut it. You have to fix the other issues before a probiotic supplement works.
Get more sleep
Sleep and gut health? Yep, you know have a reason to turn off the alarm!
The evidence of whether sleep deprivation adversely affects the microbiome is conflicting. Still, studies do show that a lack of sleep increases cortisol levels, which can affect the composition and health of your gut 17, 18.
Some research shows that chronic stress can induce dysbiosis, but it can also lead to inflammation, which is a whole other issue in and of itself.
Inflammation can cause major digestive issues like irritable bowel syndrome (IBS), small intestinal bacterial overgrowth (SIBO), celiac disease, and other health problems, in general 19, 20.
But there’s another caveat to this. Melatonin, the primary sleep hormone, is produced in the gut, so an unhealthy gut can interfere with sleep via melatonin production, and sleep deprivation can interfere with gut health, creating a nasty cycle 21.
Exercise regularly
Stress significantly impacts the gut's health and composition, and exercise is a great tool for stress management, thanks to the release of mood-boosting endorphins.
A 2018 study published in Medicine & Science in Sports & Exercise looked a the gut microbiota composition of lean and obese people who were exercising regularly and when they were sedentary 22.
Results showed that during exercise, both groups saw an increase in the diversity of microbes that produce short-chain fatty acids, which offer several health benefits for the body, including maintaining gut and immune system homeostasis 23, 24.
Researchers concluded that regular exercise could lead to compositional and functional changes in the human gut microbiota, but they are contingent on the continuation of exercise, as these changes were reversed when activity ceased.
Avoid antibiotics
Antibiotics are a standard first line of defense for many health conditions, but they’re known to kill an enormous amount of both good bacteria and bad bacteria.
If you think about the word “anti-biotic,” it’s the opposite of “pro-biotic.” The use of antibiotics, even in a single dose, can result in several negative consequences for the gut.
Antibiotics can reduce diversity of species, alter metabolic activity, and promote antibiotic-resistant organisms, leading to long-term effects like antibiotic-associated diarrhea and recurring C difficile infections 25.
Plus, exposure to antibiotics at a young age can also influence the development of diabetes or Crohn’s disease later in life 26.
When it comes to fending off bacterial infections, opt for preventative measures and natural medicine whenever possible—and if you have to take antibiotics, ensure you’re dosing up on probiotic supplements when they’re done (not during your dose) to reinstate a healthy gut microbiome.
The Takeaway
It should be obvious that virtually every aspect of your health is affected by an invisible ecosystem in your gut. While most people know diet is essential for optimal health, few people concern themselves with their gut health—and it’s not just about diet.
With disease rates skyrocketing, it’s time people start tending to it and striving for a healthy gut.
Luckily, keeping your good gut bacteria happy and healthy doesn’t have to be complicated: Eat whole high-fiber foods, load up on fermented foods, get enough sleep, exercise regularly, and supplement to fill in the gaps. Your gut and your brain will thank you.
References
- Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):3-6.
- Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474(7351):327-336.
- Kadooka Y, Sato M, Imaizumi K, et al. Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr. 2010;64(6):636-643.
- Carvalho BM, Saad MJ. Influence of gut microbiota on subclinical inflammation and insulin resistance. Mediators Inflamm. 2013;2013:986734.
- Evrensel A, Ceylan ME. The Gut-Brain Axis: The Missing Link in Depression. Clin Psychopharmacol Neurosci. 2015;13(3):239-244.
- Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021;13(3):886.
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018;9:44.
- Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Enteric Nervous System. Available from: https://www.ncbi.nlm.nih.gov/books/NBK11097/
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203-209.
- Nezami BG, Srinivasan S. Enteric nervous system in the small intestine: pathophysiology and clinical implications. Curr Gastroenterol Rep. 2010;12(5):358-365.
- Messaoudi M, Lalonde R, Violle N, et al. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr. 2011;105(5):755-764.
- Schmidt K, Cowen PJ, Harmer CJ, Tzortzis G, Errington S, Burnet PW. Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology (Berl). 2015;232(10):1793-1801.
- Roberfroid M. Prebiotics: the concept revisited. J Nutr. 2007;137(3 Suppl 2):830S-7S.
- Christ A, Lauterbach M, Latz E. Western Diet and the Immune System: An Inflammatory Connection. Immunity. 2019;51(5):794-811.
- Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006;48(4):677-685.
- Shi Z. Gut Microbiota: An Important Link between Western Diet and Chronic Diseases. Nutrients. 2019;11(10):2287.
- Zhang SL, Bai L, Goel N, et al. Human and rat gut microbiome composition is maintained following sleep restriction. Proc Natl Acad Sci U S A. 2017;114(8):E1564-E1571.
- Madison A, Kiecolt-Glaser JK. Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr Opin Behav Sci. 2019;28:105-110.
- Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014;20(39):14126-14131.
- Fakhoury M, Negrulj R, Mooranian A, Al-Salami H. Inflammatory bowel disease: clinical aspects and treatments. J Inflamm Res. 2014;7:113-120
- Chen CQ, Fichna J, Bashashati M, Li YY, Storr M. Distribution, function and physiological role of melatonin in the lower gut. World J Gastroenterol. 2011;17(34):3888-3898.
- Allen JM, Mailing LJ, Niemiro GM, et al. Exercise Alters Gut Microbiota Composition and Function in Lean and Obese Humans. Med Sci Sports Exerc. 2018;50(4):747-757.
- den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54(9):2325-2340.
- Tan J, McKenzie C, Potamitis M, Thorburn AN, Mackay CR, Macia L. The role of short-chain fatty acids in health and disease. Adv Immunol. 2014;121:91-119.
- Ramirez J, Guarner F, Bustos Fernandez L, Maruy A, Sdepanian VL, Cohen H. Antibiotics as Major Disruptors of Gut Microbiota. Front Cell Infect Microbiol. 2020;10:572912.
- Bernstein CN. Antibiotic use and the risk of Crohn's disease. Gastroenterol Hepatol (N Y). 2013;9(6):393-395.